
Sundowning symptoms affect quality of life
Someone with Alzheimer’s disease or dementia may become more agitated or anxious starting in the late afternoon and lasting through the evening and night.
They could become aggressive, delusional, paranoid, want to walk, or accidentally wander away.
Some may have disrupted sleep schedules or restlessness at night.
This behavior is called dementia sundowning because it typically begins around sundown – late afternoon or evening.
These dementia sundowning symptoms negatively affect your older adult’s quality of life and are challenging for you to manage.
We explain what causes sundowning and share 7 ways to manage the symptoms and behaviors. These suggestions make evenings calmer and easier for both your older adult and you.
What causes dementia sundowning?
Some studies show that sundowning affects up to 20% of people with Alzheimer’s. And, it can also affect older adults who don’t have dementia.
Researchers don’t know exactly why sundowning happens, but think that it’s caused by the changes in the brain due to dementia.
The body clock, which regulates when we’re awake and when we’re asleep, might be affected by those changes.
7 ways to reduce and manage sundowning symptoms
1. Go along with their reality
Sometimes, a person with dementia will experience a different time in their lives, like when they were parents of young children, going to work, waiting for their parents as a child, or something familiar from their past.
If this happens, do your best to go along with their reality. Trying to force them back into our reality won’t work and will only cause upset or anger.
It may help to engage them in an activity that’s similar to what’s happening in their mind.
For example, if they’re waiting for someone to come home, do something they would have done in that real situation. Maybe they would be making a snack, preparing dinner, or straightening up the house.
Think about their routines and activities when they were younger and brainstorm activities that would fit the situations that feel familiar to them.
Later, if needed, you could use a therapeutic fib to transition out of that activity and redirect their attention somewhere else.
For example, if they’re waiting for their mom to pick them up from school, you could help them get ready by gathering up their school bag, using the toilet, and getting their jacket.
If doing that slowly isn’t enough of a distraction to transition to another activity, you could say that their mom called and said she would be a bit late so she asked that they went ahead and had a snack while waiting.
During and after the snack, you’ll have more opportunities to transition to other enjoyable activities.
2. Listen carefully to understand the emotions behind their words
When someone is having sundowning symptoms, they may make strange requests, like asking for their mother or to go home.
Even if their words don’t make logical sense, listen for and respond to the emotion behind the words.
In some cases, they could be trying to express fear or loneliness. In other cases, they might be expressing frustration, discomfort, anger, or other emotions.
If your older adult is going through some tough emotions, they may not be ready to change how they feel.
It may be kinder and more effective to support them while they take time to process their emotions. You can do that by showing that you’re on their side.
Some people might like you to sit with them, hold their hand, or give hugs. Others may simply like your company nearby or for you to be a sympathetic listener.
Neutral, but supportive, responses could include:
- I understand.
- That’s a lot to deal with.
- Oh, that must be hard.
- Of course you miss your Mom.
4. Create safe spaces where they can move around
Some people get restless and want to move around. If your older adult wants to walk or pace, create a safe area for them to do so.
This could be a clear path somewhere in the house or a safe area in a secure backyard where you can keep an eye on them.
They may also appreciate having you walk with them so they won’t feel alone as they move around.
5. Engage them in calming activities
Engaging someone with dementia in calming, soothing activities is a positive way to direct their energy.
An activity that they enjoy and makes them feel good helps them focus on something other than boredom, fear, anxiety, or frustration.
Create a space in a calming environment for them to focus on this activity.
Some people like repetitive activities like sorting papers, folding laundry (small towels), shuffling cards, etc.
Some may enjoy listening to soothing music, coloring, painting, cuddling a baby doll or stuffed animal.
Try different activities to see which they like best and which are most calming.
6. Create a pre-bedtime wind down routine
It can be tough for someone with dementia to go from the normal activities of daily life directly to lying down and quickly falling asleep within 30 minutes. (Many caregivers struggle with this too.)
To smooth the transition and make it easier to settle down and go to sleep, add a pre-bedtime wind down routine.
This is a time when you make the environment extra calm and soothing to help older adults relax and slow down.
For example, turn off the TV or switch to a non-exciting show played at a low volume. If music is playing, make it soft, soothing, and at a low volume. Consider using aromatherapy to scent the air with a relaxing scent like lavender.
Some people may enjoy hearing a book read aloud, looking at photos that remind them of happy times, or sitting quietly with an activity.
If there are activities they enjoy and usually calm them, this is a great time for those options.
Lighting can be a bit tricky, so experiment to find out what works best.
Typically, dimming the lights a little helps to transition from activity to sleep. But with sundowning, shadows or dark corners can provoke anxiety or hallucinations.
Do your best to find a level of lighting that’s dimmer than usual, but not so dim that shadows start playing tricks on their eyes.
7. Consider medication
In some cases of sundowning, especially when these and other non-drug methods of reducing symptoms don’t work, it may be helpful to try medication.
Work with their doctor to experiment carefully with medications.
Some medications may actually disrupt sleep patterns and energy levels in a way that makes sundowning worse, not better.
Next Step Find out about 7 additional ways to reduce dementia sundowning symptoms
Recommended for you:
- 7 Ways to Reduce Dementia Sundowning Symptoms
- 3 Top Benefits of a Daily Routine for Seniors
- Keeping a Dementia Journal Makes Caregiving Easier: 7 Things to Track
By DailyCaring Editorial Team
[optin-monster slug=”yxbytm35zhsdfopnw7qk”][optin-monster slug=”jvhyplxmb4umsjazxecn”]
About the Author

Connie Chow
Connie was a hands-on caregiver for her grandmother for 20 years. (Grandma made it to 101 years old!) She knows how challenging, overwhelming, and all-consuming caring for an older adult can be. She also knows how important support is — especially in the form of practical solutions, valuable resources, and self-care tips.




Yes, every evening I leave my loved one a checklist something like this, even if I’m staying home— and he actually checks the boxes! Good night, Sweetheart. I’ll be home after midnight [ ] dinner is beef and broccoli [ ] dessert is tapioca and blueberries [ ] Rebecca will be here from 6 to 10 [ ] take your Tuesday night pills before you go to bed [ ] virtual hug and kiss good night! PS: we picked up all the newspapers and mail already.
This is great! Thanks for sharing what’s been working for you both.
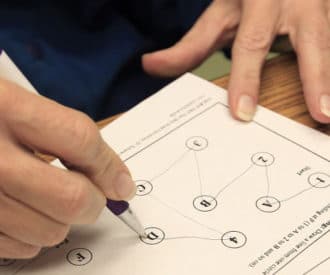
Has anyone used a visual schedule that shows the bedtime routine so your loved one know what to expect that evening? These kinds of visuals are used successfully with students who have cognitive challenges to manage behaviors.
I personally experienced something like “sundowning” when my second child was born. I became anxious in early evenings because I did not know what my night would be like!
A visual schedule is a good idea to try! Thanks for the suggestion.