What if some of the very pills meant to help manage common age-related ailments could be stealthily harming your loved one's brain? This isn't a medical mystery, but a critically important risk that many families are unaware of.
A specific class of medications, known as anticholinergics, has been linked to worsening dementia symptoms and even increasing the long-term risk of cognitive decline. From over-the-counter sleep aids to certain prescription drugs, these medications are more common than you might think.

Understanding this connection is a decisive step in protecting your loved one's cognitive health and ensuring their treatment plan is truly safe.
Common Medications That Can Cause Dementia Symptoms
Standard prescription and over-the-counter medications called anticholinergics (anti-col-in-er-jik; hear it) have side effects that can worsen existing Alzheimer’s disease or dementia symptoms.
This type of drug can even cause dementia-like symptoms in people without cognitive impairment.
We explain:
- Why do these medications cause dementia symptoms
- How do they increase the risk of dementia
- Which medications are anticholinergics
- Common cognitive and physical side effects
- What to do if your older adult is currently taking these meds
Important: NEVER start, stop, or adjust the dosage for any medications without asking your older adult’s doctor for advice – that can cause serious health problems.
Why Do Anticholinergics Cause Dementia Symptoms?
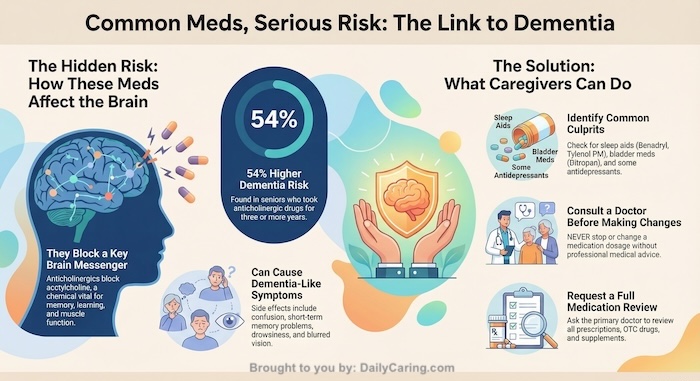
Anticholinergics block acetylcholine, a neurotransmitter (brain chemical) that’s used for learning, memory, and muscle functions.
You can think of neurotransmitters as messengers that carry instructions within the brain and from the brain to the rest of the body.
Older adults already have fewer of these messengers because our bodies produce less of this neurotransmitter as we age.
On top of that, blocking it with drugs makes it even harder for instructions to get delivered.
If instructions aren’t getting delivered, the brain and body won’t be able to work correctly.
This causes dementia symptoms to worsen or even to start showing up in seniors without dementia.
INFOGRAPHIC: Medications Linked to Dementia
Anticholinergic Drugs Can Increase Dementia Risk by 54%
Seniors who don’t have Alzheimer’s or dementia still need to be careful of anticholinergic medications.
That’s because these drugs can increase the risk of developing dementia in the future.
A study of adults aged 65+ found that those who took an anticholinergic drug for three or more years (or in high doses for a shorter time) had a 54% higher dementia risk.
Which Medications Have Anticholinergic Properties?
Many common prescription and over-the-counter (OTC) medications have anticholinergic effects that can worsen dementia symptoms or increase the long-term risk of cognitive decline. Often, people are unaware that everyday products contain these compounds.
To help you understand which prescription and over-the-counter drugs have anticholinergic effects, we found a helpful list that specifies the drugs with “definite” vs. “possible” anticholinergic activity.
Work with their doctor to focus on minimizing drugs in the “definite” category.
Medical conditions include a wide variety of common issues like overactive bladder, sleep issues, coughs, colds, allergies, behavior issues, mood disorders, chronic obstructive pulmonary disease (COPD), and Parkinson’s disease.
Common Anticholinergic Medications Include:
OTC Sleep Aids and Antihistamines: The main ingredient is often diphenhydramine, found in products like Benadryl, Tylenol PM, and Unisom. Other examples include doxylamine.
Overactive Bladder (OAB) Medications: These are frequently prescribed and include drugs like oxybutynin (Ditropan), tolterodine (Detrol), and solifenacin (Vesicare).
Tricyclic Antidepressants (TCAs): Older antidepressants are strongly anticholinergic, with examples like amitriptyline (Elavil) and doxepin (Sinequan).
Muscle Relaxants: Drugs such as cyclobenzaprine (Flexeril) also have anticholinergic properties.
This list might not include every condition or medication, but it’s a good start for finding out whether any of your older adults’ medications are anticholinergics.
Use this list to have an informed conversation with your older adult’s doctor about the risks and benefits of taking that medication.
VIDEO: Understanding Anticholinergics and Dementia Risk
If You Have More Questions, Consult “The Beers List”
The American Geriatrics Society Beers Criteria® (The Beers List) identifies many of these medications, particularly those with strong anticholinergic properties, as potentially inappropriate for older adults due to the heightened risk of adverse effects like confusion, cognitive impairment, and delirium. Consulting your loved one's doctor or pharmacist with this list is a crucial step in reviewing their medication regimen and finding safer alternatives.
What Are the Common Side Effects of Anticholinergic Medications?
In addition to blocking neurotransmitters, anticholinergic drugs also have side effects.
Cognitive side effects include:
- Confusion
- Problems with short-term memory
- Problems with reasoning
Physical side effects include:
- Blurred vision
- Drowsiness
- Easily overheating
- Dry mouth
- Constipation/urine retention
These side effects can make existing dementia symptoms worse or make someone without cognitive issues behave as if they have Alzheimer’s or dementia.
What Should You Do if Your Loved One is Taking Anticholinergic Medications?
Important: NEVER start, stop, or adjust the dosage for any medicines without asking your older adult’s doctor for advice – that can cause serious health problems.
The first step is to discuss any medication concerns with the doctor as soon as possible. Ask them to explain the risks and benefits and make a recommendation.
Because many seniors have multiple health conditions, they may be taking more than one type of anticholinergic medication.
One anticholinergic drug might not be harmful, but the side effects and doses can add up across different medications.
That’s why it’s so essential for a doctor to review all the medications that your older adult takes.
And if other doctors are prescribing different drugs, ask your primary physician to review the complete medication list, including over-the-counter medicines and supplements.
This could also be a good opportunity for the doctor to discontinue drugs that are no longer needed safely.
Final Thoughts About Anticholinergics and Dementia Risk
Knowledge is your greatest defense. This information isn't meant to cause panic, but to empower you to have a proactive, informed conversation with your loved one's doctor. By reviewing their medication list through this critical lens, you become an essential partner in safeguarding their brain health.
It’s a profound act of care to question, “Is this medication still necessary, or is there a safer alternative?” Asking these questions could protect their memory, clarity, and quality of life, ensuring their medications are part of the solution—not an unseen part of the problem.
*This post is for information purposes only. Always consult your physician or healthcare professional before making any changes to your medication management routine.
Next Steps: Check the list of common anticholinergic medications
Recommended for you:
- The Beers List: Medications Seniors Should Use with Caution
- 10 Medications That Cause Falls in Seniors: Use with Caution
- 5 Tips for Choosing the Safest Over-the-Counter Painkillers for Seniors
About the Author

Connie is the founder of DailyCaring.com and was a hands-on caregiver for her grandmother for 20 years. (Grandma made it to 101 years old!) She knows how challenging, overwhelming, and all-consuming caring for an older adult can be. She also understands the importance of support, especially in the form of practical solutions, valuable resources, and self-care tips.














Thank you!
You’re very welcome!
I have been suffering from early onset Alzheimer’s for the last 3.5 years. I turned 43 in July and now I am at the mid stages of Alzheimer’s. Every website that I come says it’s for seniors. Does anybody know A website or group that I can relate to you better? With people my age that has Alzheimer’s? I appreciate any info.
We found a section on the Alzheimer’s Association website that’s dedicated to Younger/Early-Onset Alzheimer’s. These pages might be helpful (the first link includes a list of additional resources):
– https://www.alz.org/alzheimers-dementia/what-is-alzheimers/younger-early-onset
– https://www.alz.org/help-support/i-have-alz/younger-onset
We also found a few other resources that might be helpful:
– https://my.clevelandclinic.org/health/articles/9592-living-with-early-onset-alzheimers-disease
– https://www.beingpatient.com/early-onset-alzheimers-5-signs/
– https://www.hopkinsmedicine.org/health/conditions-and-diseases/alzheimers-disease/earlyonset-alzheimer-disease
– https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers/art-20048356