For an older adult with limited mobility, these injuries can develop silently and rapidly, often hidden beneath clothing or bedding.
Yet, with awareness and vigilance, they are largely preventable. Understanding the “why” and “when” of their formation is the first, most critical step in protecting your loved one's comfort and health.
Let’s explore the causes, stages, and most importantly, the life-changing power of early detection to keep their skin safe and healthy.

Seniors with limited mobility are at serious risk for bed sores (pressure sores). Spending a significant amount of time sitting or lying down without changing position can lead to these potentially life-threatening wounds. Vive Health explains why bed sores are so deadly, their causes, stages, and how to detect them before severe damage occurs.
If you are caring for an older adult with limited mobility or confined to a bed, recliner, or wheelchair, knowing how to recognize bed sores is a must.
Bed Sores Can Progress and Become Debilitating if Not Treated Properly
While seemingly harmless at first, bed sores can quickly progress to life-threatening tissue decay and infection.
It may sound dramatic, but whisper concerns about a bed sore to any medical professional, and they’ll probably have a wound care specialist evaluating your older adult STAT.
Unfortunately, the people most susceptible to developing bed sores are the ones already experiencing debilitating illnesses, which have cost them their mobility in the first place.
Find out what a bed sore is, what causes them, the four stages of bed sore severity, and how to spot one before it turns into a severe wound.
What is a Bed Sore?
Bed sores, also known as pressure sores or pressure ulcers, are open wounds on the body where skin and tissue are breaking down due to prolonged pressure from underlying bones.
When someone spends most of their time lying or sitting in the same position, the body's bony protrusions can put pressure on internal tissues.
Over time, this disrupts blood circulation, leading to tissue damage and skin breakdown.

Common bed sore locations include:
- Shoulder blades
- Tailbone
- Hips
- Elbows
- Heels
VIDEO: All About BedSores: Prevention and Care
What Causes Bed Sores? 7 Contributing Factors
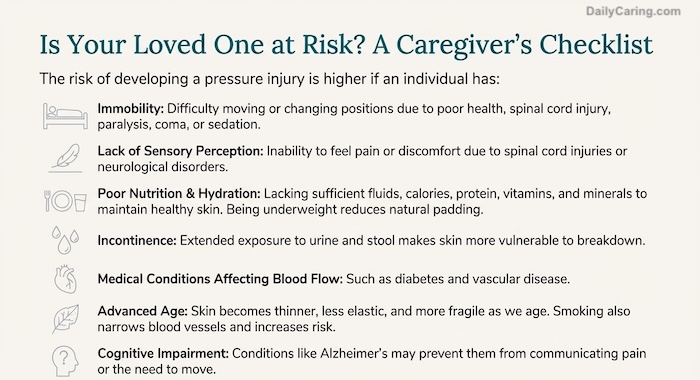
1. Lack of movement
Advanced age or severe health conditions can reduce an older adult’s mobility. And, if they’re also affected by paralysis, coma, sedation, or injury, that will force them to lie down or sit for long periods of time.
This significantly increases the risk of developing bed sores.
2. Older age
As we age, our skin becomes thinner and less elastic. The loss of skin strength makes older adults who spend most of their time sitting or lying down more vulnerable to sores.
3. Poor nutrition
Essential vitamins and minerals play a critical role in maintaining the strength of skin and tissues. Those include protein, vitamin C, zinc, calcium, and potassium.
If an older adult’s diet is missing whole foods that aid tissue repair and support blood circulation, they could be at higher risk for skin breakdown and bed sores.
4. Being underweight
Many patients with chronic illness, especially those who may be underweight because of loss of appetite, dysphagia (difficulty swallowing), or medication side effects.
Unfortunately, the less fat and padding there is on the body, the less able it is to protect against pressure from bony protrusions, and the more likely it is to develop a bed sore.
5. Smoking
Smoking leads to heart disease and cancer, and it also increases the risk of bed sores.
That’s because it narrows blood vessels, which decreases circulation. Then, vulnerable tissues don’t receive the oxygen and nutrients they need from the poorly circulating blood.
6. Incontinence
Contact with urine and feces from incontinence can make the tailbone and even hip areas more susceptible to skin breakdown.
The skin will be more easily broken and in close contact with bacteria.
7. Cognitive impairment
Suppose your older adult has Alzheimer’s disease, dementia, or another cognitive decline that affects their ability to communicate. In that case, they may have difficulty alerting you to or describing pain from a developing bed sore.
VIDEO: Conducting a Skin Assessment: Preventing Bed Sores in Hospitals
The 4 Stages of Bed Sores
There are four main stages of bed sores, which range from initial warning signs to life-threatening tissue decay.
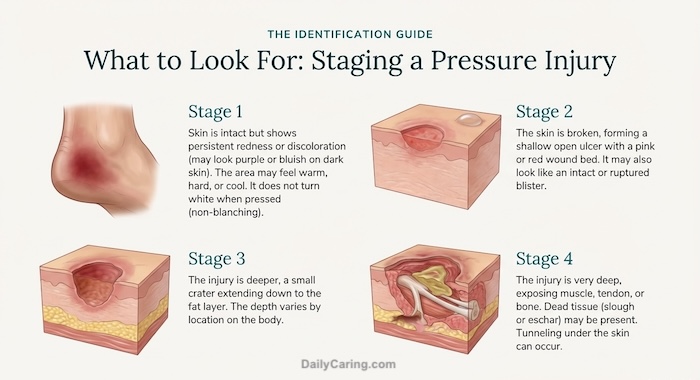
Bed Sores: Stage I
Slight to significant redness and discoloration of the skin at a bony pressure point is the first warning sign that a bed sore is developing.
To test for a potential bed sore, find out if the area “blanches.” If it does, the tissue hasn’t been damaged yet.
To test, lightly press the spot with your finger. If it goes white and then flushes red again, it is successfully blanching. Try it on yourself to see what the non-damaged reaction looks like.
Bed Sores: Stage II
Left unmonitored and untreated, a bed sore will progress to where the skin breaks open and the beginnings of an ulcer form. The area will feel tender and painful to your older adult.
Bed Sores: Stage III
A stage III bed sore forms a deep crater through skin and layers of tissue to the subcutaneous fat underneath. The less blood flow the area gets, the more tissue that decays.
Bed Sores: Stage IV
In the final stage, a bed sore has progressed so far that the ulcerous crater goes all the way down through the soft tissue to show bone.
This massive breakdown and decay are at extremely high risk for infection and are a life-threatening condition.
How to Detect a Bed Sore
Paying attention to an older adult’s body helps you prevent bed sores or spot them early.
Every day, scan their body and double-check the bony parts for discolorations. Do the blanch test on any suspicious areas. Ask your loved one if they have pain or discomfort anywhere.
Common signs of developing bed sores:
- Unusual changes in skin color or texture
- Swelling
- Pus-like draining
- Skin that feels cooler or warmer to the touch than other areas
- Tender areas
What Should I Do If a Bed Sore is Suspected?
If you’re worried about a potential bed sore, get your loved one a medical exam right away – sores can develop and worsen significantly within days.
How to Prevent Bed Sores: The 3 Pillars of Prevention
- Consistent Repositioning
- Proactive Skin Care
- Foundational Nutrition

Final Thoughts About Bed Sores in Aging Adults
Protecting a loved one from bed sores is a profound act of daily care and attention. By knowing what to look for and taking simple, consistent preventive measures, you are actively guarding your loved one's comfort and dignity.
Early detection is your most effective tool. It transforms a potentially severe health crisis into a manageable condition. Remember, your watchful eye and gentle care make all the difference.
With this knowledge, you can ensure their skin remains healthy, helping them rest more easily and live more comfortably.
*This post is for informational purposes only. If you suspect a bed sore or any other medical issue in your loved one, contact a medical professional immediately.
Next Steps: Get 3 tips for preventing bed sores and find out about the 2 methods doctors typically use to treat them
Recommended for you:
- 6 Hygiene Tips for Bed Bound Seniors
- Incontinence Care: 9 Tips for Caregivers
- 10 Common Chronic Diseases in Seniors: How to Prevent and Manage
About the Author
Jessica Hegg is a manager at ViveHealth.com. Ms. Hegg was also a full-time caregiver for her Mom who had Primary Progressive MS and Epilepsy. She is a freelance writer with a passion for cooking and lives in Austin, TX with her Mom and her wonderful husband. You can find her personal blog about caregiving tips, ideas, and solutions at Givea.Care.