Keeping an aging adult’s teeth and mouth healthy can be challenging because aging and health conditions can make them more vulnerable to dental problems. Corson Dental shares expert tips on preventing, treating, and managing common dental problems in older adults.
Wisdom may come with age, but so do a multitude of problems associated with aging teeth and gums.
A lifetime of chewing, grinding, gnashing, and general wear and tear combined with medications, medical conditions, and a potential decrease in dental care can cause many oral health problems in older adults.
These issues may result in significant tooth pain, inflamed gums, bleeding gums, or gum infection.
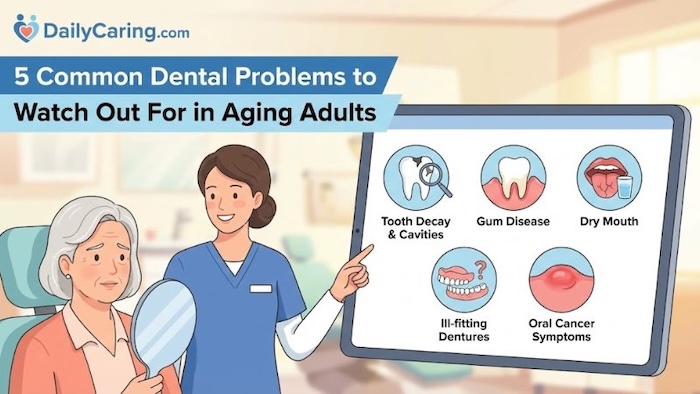
Here are 5 common geriatric dental problems to watch out for, plus advice on prevention, treatment, and management.
5 Common Dental Problems to Watch Out For in Aging Adults
1. Tooth decay
Tooth decay can lead to cavities, which can cause pain, infection, and even tooth loss. It is often caused by a build-up of plaque and tartar.
A diet high in sugary foods, a tendency to snack between meals, and decreased saliva production all contribute to the buildup of sugar and acid in the mouth.
Medical conditions can play a major role, too. For example, tooth brushing can be difficult and painful for those with arthritis and can seem near impossible for those with dementia.
Prevention is the best approach. Brush teeth twice a day with fluoride toothpaste, reduce intake of sugary foods, and drink water after each meal. Switching to an electric toothbrush may be easier to use and is more effective.
If tooth decay remains a concern, talk to the dentist about options such as fluoride rinses or fillings and crowns to address advanced decay.
2. Gum disease
Gum disease, also called periodontal disease, is a common problem caused by bacteria in plaque and tartar. Smoking can also play a significant role. Symptoms in the later stages of gum disease include irritated, red, and bleeding gums.
Gingivitis is the inflammation of the gums due to bacterial buildup where the teeth meet the gum tissue. This can develop into periodontitis, a serious gum infection that damages the gum tissue and the bone that supports the teeth.
If the ability to chew and swallow is impaired, inadequate nutrition can also lead to additional gum health issues.
Thankfully, gum disease is both preventable and treatable through proper dental care. This includes flossing and brushing daily.
Definitely visit the dentist if your older adult has symptoms of gum disease. They’ll be able to provide a detailed assessment and evaluation and create a treatment plan.
3. Receding gums
Gum recession is a gradual process in which the gums shrink away from the teeth. It is commonly caused by gum diseases and poor dental hygiene, although smoking, family history, and teeth grinding (known as bruxism) are also possible contributing factors.
Teeth may become sensitive as the root becomes exposed, and they may appear to lengthen. Untreated, this condition can result in significant damage to oral tissues, an increased likelihood of developing gum disease, and tooth loss.
Again, prevention is the best cure, through practising good oral hygiene, quitting smoking, and avoiding sugary foods.
If your older adult shows signs of receding gums, visit the dentist as soon as possible to discuss the best approach to address the issue. Treatment options range from deep cleaning or scaling to surgical procedures such as gum grafts.
4. Dry mouth
Many people experience decreased saliva production with age, a common condition known as dry mouth (xerostomia). It is also a known side effect of many medications.
The problem with reduced saliva production is that sugar and acids build up more readily in the mouth, increasing the risk of cavities and leading to some of the problems mentioned above. It can also result in dry, cracked lips and a swollen tongue, making it difficult to speak and swallow.
To combat these negative consequences, have your older adult drink water regularly and avoid sugary foods and drinks. Chewing gum and lozenges can stimulate saliva production, and mouth rinses can prevent acid build-up.
5. Oral cancer
The chance of oral cancer increases with age. People who smoke or drink alcohol frequently are at higher risk.
It is worthwhile to have the dentist check out any persistent sores, ulcers, or color changes in the tissue in or around your older adult’s mouth.
Early identification could save your older adult’s life, so regular dental examinations are important to ensure that their gums and surrounding tissue are as healthy as possible.
Comparison Table: At-a-Glance Guide for Dental Issues Facing Seniors
Final Thoughts on Dental Issues Facing Seniors
Maintaining good oral health in older adults requires consistent care and professional support. Regular dental check-ups are essential for early detection and management of common issues like tooth decay and gum disease.
Addressing these problems promptly not only preserves natural teeth but also contributes to overall comfort, nutrition, and well-being. By committing to diligent daily hygiene and partnering with dental professionals, seniors can enjoy a healthier, more confident smile for years to come.
Frequently Asked Questions
Caregiving comes with unique challenges regarding oral hygiene. Below are answers to the most common questions families ask about senior dental care.
The information provided in this article, including text, graphics, and images, is for informational and educational purposes only. It is not intended to be a substitute for professional dental or medical advice, diagnosis, or treatment. Always seek the advice of your dentist, physician, or other qualified health provider with any questions you may have regarding a medical condition or dental health concerns. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recommended for you:
- How to Help Someone with Alzheimer’s Brush Their Teeth
- 3 Ways to Improve Senior Dental Health and Reduce Heart Disease and Alzheimer’s Risk
- How Often Should Seniors Bathe? 3 Essential Health Tips
Guest contributor: Corson Dental is a dental practice located in Tauranga, New Zealand. Corson uses advanced technologies to help clients achieve a beautiful, healthy smile, with options ranging from simple preventive treatments to specialised cosmetic procedures.
This article contains affiliate links. We never link to products or services for the sole purpose of making a commission. For more information, see How We Make Money.
About the Author

Connie is the founder of DailyCaring.com and was a hands-on caregiver for her grandmother for 20 years. (Grandma made it to 101 years old!) She knows how challenging, overwhelming, and all-consuming caring for an older adult can be. She also understands the importance of support, especially in the form of practical solutions, valuable resources, and self-care tips.














Unpleasant taste of mouth
If there are no dental issues causing an unpleasant taste in the mouth, it might be a good idea to speak with the doctor to find out if any health conditions or current medications could cause that to happen.